ANDOVER, Mass. — The liquid that many hope could help end the Covid-19 pandemic is stored in a nondescript metal tank in a manufacturing complex owned by Pfizer, one of the world’s biggest drug companies. There is nothing remarkable about the container, which could fit in a walk-in closet, except that its contents could end up in the world’s first authorized Covid-19 vaccine.
Pfizer, a 171-year-old Fortune 500 powerhouse, has made a billion-dollar bet on that dream. So has a brash, young rival just 23 miles away in Cambridge, Mass. Moderna, a 10-year-old biotech company with billions in market valuation but no approved products, is racing forward with a vaccine of its own. Its new sprawling drug-making facility nearby is hiring workers at a fast clip in the hopes of making history — and a lot of money.
In many ways, the companies and their leaders couldn’t be more different. Pfizer, working with a little-known German biotech called BioNTech, has taken pains for much of the year to manage expectations. Moderna has made nearly as much news for its stream of upbeat press releases,
executives’ stock sales, and spectacular rounds of funding as for its science.
Each is well-aware of the other in the race to be first.
But what the companies share may be bigger than their differences: Both are banking on a genetic technology that has long held huge promise but has so far run into biological roadblocks. It is called
synthetic messenger RNA, an ingenious variation on the natural substance that directs protein production in cells throughout the body. Its prospects have swung billions of dollars on the stock market, made and imperiled scientific careers, and fueled hopes that it could be a breakthrough that allows society to return to normalcy after months living in fear.
There are about a
dozen experimental vaccines in late-stage clinical trials globally, but the ones being tested by Pfizer and Moderna are the only two that rely on messenger RNA.
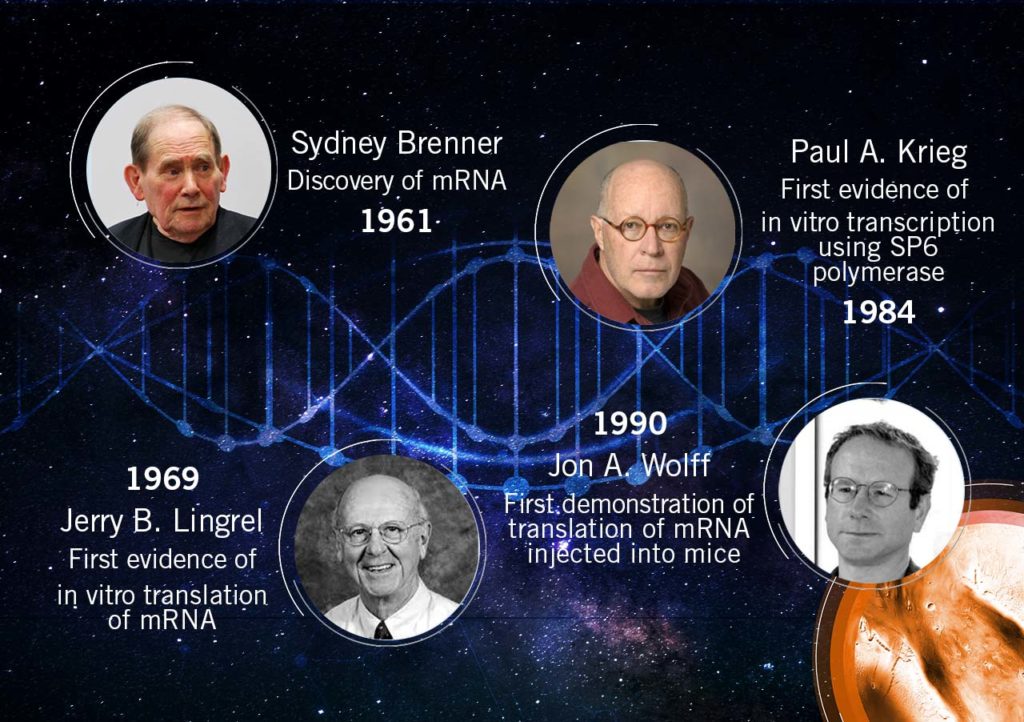
For decades, scientists have dreamed about the seemingly endless possibilities of custom-made messenger RNA, or mRNA.
Researchers understood its role as a recipe book for the body’s trillions of cells, but their efforts to expand the menu have come in fits and starts. The concept: By making precise tweaks to synthetic mRNA and injecting people with it, any cell in the body could be transformed into an on-demand drug factory.
But turning scientific promise into medical reality has been more difficult than many assumed. Although relatively easy and quick to produce compared to traditional vaccine-making, no mRNA vaccine or drug has ever won approval.
Even now, as Moderna and Pfizer test their vaccines on roughly 74,000 volunteers in pivotal vaccine studies, many experts question whether the technology is ready for prime time.
“I worry about innovation at the expense of practicality,” Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine and an authority on vaccines, said recently. The U.S. government’s
Operation Warp Speed program, which has underwritten the development of Moderna’s vaccine and pledged to buy Pfizer’s vaccine if it works, is “weighted toward technology platforms that have never made it to licensure before.”
Whether mRNA vaccines succeed or not, their path from a gleam in a scientist’s eye to the brink of government approval has been a tale of personal perseverance, eureka moments in the lab, soaring expectations — and an unprecedented flow of cash into the biotech industry.
It is a story that began three decades ago, with a little-known scientist who refused to quit.
Before messenger RNA was a multibillion-dollar idea, it was a scientific backwater. And for the Hungarian-born scientist behind a key mRNA discovery, it was a career dead-end.
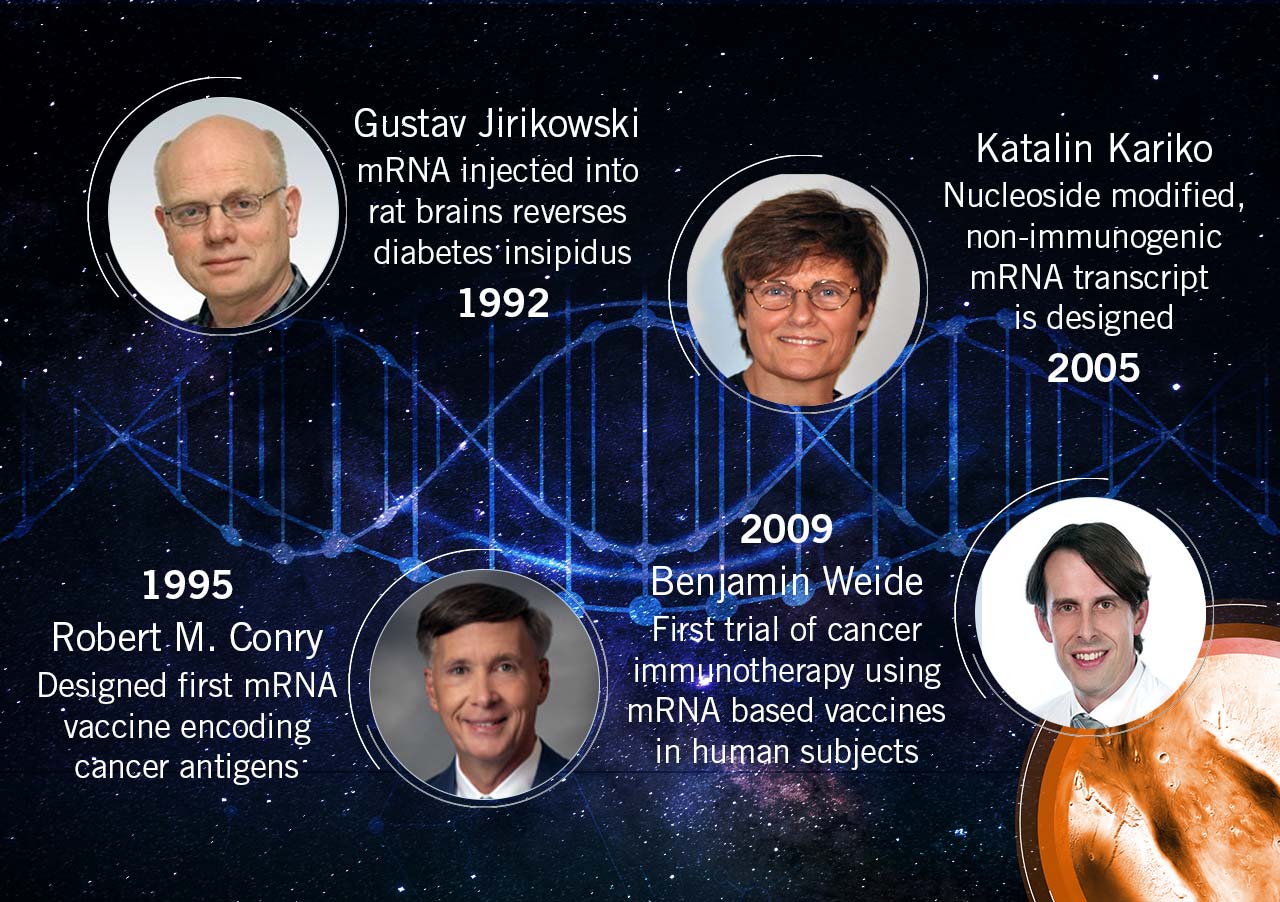
Katalin Karikó spent the 1990s collecting rejections. Her work, attempting to harness the power of mRNA to fight disease, was too far-fetched for government grants, corporate funding, and even support from her own colleagues.
It all made sense on paper. In the natural world, the body relies on millions of tiny proteins to keep itself alive and healthy, and it uses mRNA to tell cells which proteins to make. If you could design your own mRNA, you could, in theory, hijack that process and create any protein you might desire — antibodies to vaccinate against infection, enzymes to reverse a rare disease, or growth agents to mend damaged heart tissue.
In 1990, researchers at the University of Wisconsin managed to
make it work in mice. Karikó wanted to go further.
The problem, she knew, was that synthetic RNA was notoriously vulnerable to the body’s natural defenses, meaning it would likely be destroyed before reaching its target cells. And, worse, the resulting biological havoc might stir up an immune response that could make the therapy a health risk for some patients.
It was a real obstacle, and still may be, but Karikó was convinced it was one she could work around. Few shared her confidence.
“Every night I was working: grant, grant, grant,” Karikó remembered, referring to her efforts to obtain funding. “And it came back always no, no, no.”
By 1995, after six years on the faculty at the University of Pennsylvania, Karikó got demoted. She had been on the path to full professorship, but with no money coming in to support her work on mRNA, her bosses saw no point in pressing on.
She was back to the lower rungs of the scientific academy.
“Usually, at that point, people just say goodbye and leave because it’s so horrible,” Karikó said.
There’s no opportune time for demotion, but 1995 had already been uncommonly difficult. Karikó had recently endured a cancer scare, and her husband was stuck in Hungary sorting out a visa issue. Now the work to which she’d devoted countless hours was slipping through her fingers.
“I thought of going somewhere else, or doing something else,” Karikó said. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
In time, those better experiments came together. After a decade of trial and error, Karikó and her longtime collaborator at Penn — Drew Weissman, an immunologist with a medical degree and Ph.D. from Boston University — discovered a remedy for mRNA’s Achilles’ heel.
The stumbling block, as Karikó’s many grant rejections pointed out, was that injecting synthetic mRNA typically led to that vexing immune response; the body sensed a chemical intruder, and went to war. The solution, Karikó and Weissman discovered, was the biological equivalent of swapping out a tire.
Every strand of mRNA is made up of four molecular building blocks called nucleosides. But in its altered, synthetic form, one of those building blocks, like a misaligned wheel on a car, was throwing everything off by signaling the immune system. So Karikó and Weissman simply subbed it out for a slightly tweaked version, creating a hybrid mRNA that could sneak its way into cells without alerting the body’s defenses.
“That was a key discovery,” said Norbert Pardi, an assistant professor of medicine at Penn and frequent collaborator. “Karikó and Weissman figured out that if you incorporate modified nucleosides into mRNA, you can kill two birds with one stone.”
That discovery, described in a series of scientific papers starting in 2005, largely flew under the radar at first, said Weissman, but it offered absolution to the mRNA researchers who had kept the faith during the technology’s lean years. And it was the starter pistol for the vaccine sprint to come.
And even though the studies by Karikó and Weissman went unnoticed by some, they caught the attention of two key scientists — one in the United States, another abroad — who would later help found Moderna and Pfizer’s future partner, BioNTech.